Erysipelas In Childhood

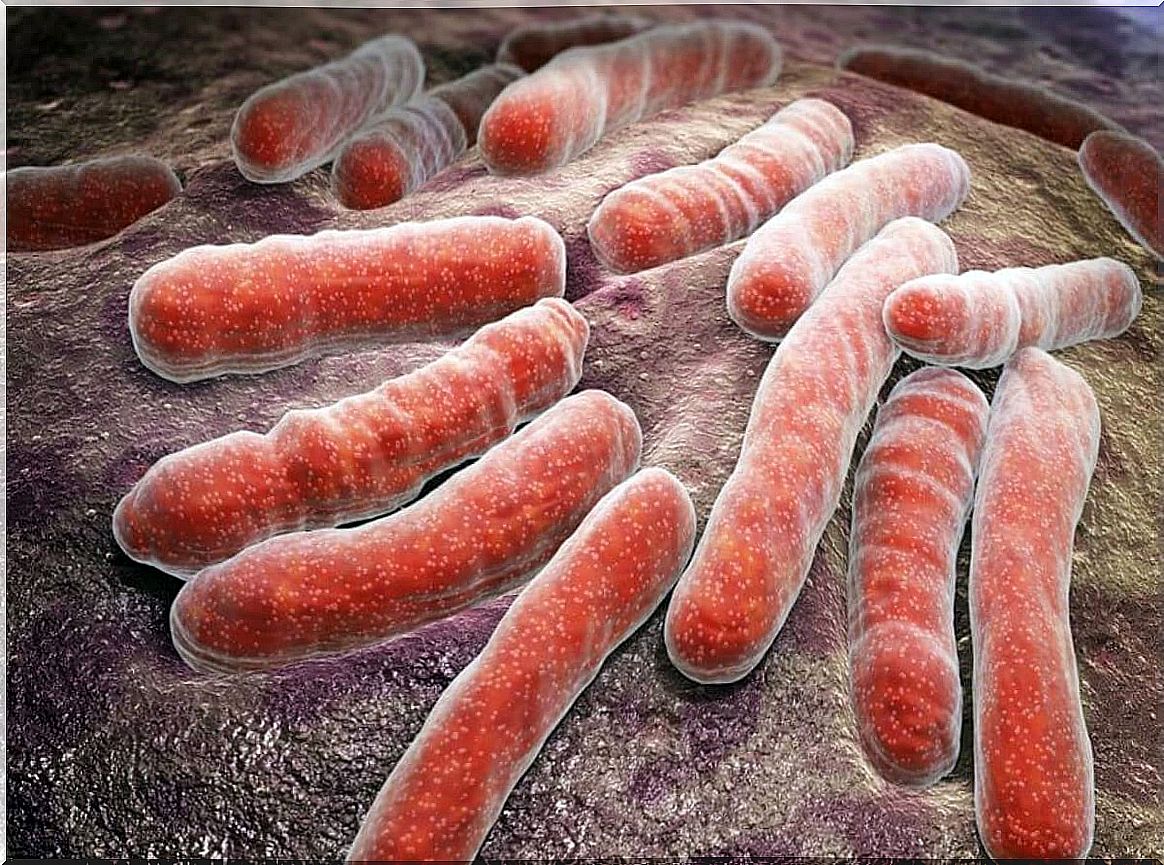
Erysipelas in childhood is one of the great reasons for hospitalization and morbidity. It is even a very common cause in pediatric primary care consultations. The origin in most cases of erysipelas is caused by bacterial infectious pictures that affect the epidermis and the superficial dermis.
The cause of erysipelas in childhood
Erysipelas is a skin infection that affects the epidermis and papillary dermis. However, it can spread to the superficial skin lymph nodes.
In the majority of cases in which they occur on the face (5 to 20%) they are due to group A beta hemolytic Streptococcus , known as S treptococcus pyogenes . While the etiology of the lower extremities (80% of cases) is related to other Streptococcus of group B, C or G.
Skin fissures are the first step in the genesis of this pathology. Thus, there are multiple entry gates to inoculate the bacteria and proliferate:
- Surgical incisions.
- Insect bites.
- Small wound.
- Stasis ulcers.
- Chickenpox scratching lesions.
The infection spreads and directly invades the lymphatic system and causes disease.
Clinical manifestations
When making the diagnosis of erysipelas, the child should be examined for skin trauma or recent episodes of pharyngitis.
Local demonstrations
It is characterized by a reddened skin region that is well defined and raised, according to a review published in The New England Journal of Medicine . It most often affects the lower extremities and then the face
In most cases it relates local signs such as the following:
- Pain.
- Lymphangitis
- Regional adenopathy.
In turn, children with erysipelas may complain of burning or tenderness and itching in the area of infection.
General manifestations
The general symptoms can vary according to the severity. However, the most frequent signs are those detailed below:
- Fever.
- Leukocytosis with neutrophilia.
- Increase in acute phase reactants (increase in C-reactive protein).
One of the possible entry points may be the presence of a mycosis, for which the interdigital spaces of the fingers should be examined in search of maceration, desquamation or fissures.
The differential diagnosis is made with infectious cellulitis. In fact, infectious cellulitis has poorly defined borders and its evolution is slower.
Complications of erysipelas
Erysipelas can develop a serious infectious picture, but it is rarely fatal. Consequently, the most serious pathology manifests itself with blisters, vesicles, even obvious necrosis.
Some of the more relevant local complications include the following:
- Abscesses
- Scarlet fever.
- Pneumonia.
- Meningitis.
- Skin necrosis.
- Hemorrhagic purpura.
- Thrombophlebitis.
- Blistering
Treatment options for erysipelas in childhood
When the infectious picture is suspected to be erysipelas, treatment with antibiotics against Streptococcus should be started .
Oral antibiotics
The first line of treatment for this disease is penicillin or its semisynthetic derivatives, the way it is administered will depend on the severity of the clinical picture. This is recommended by the 2014 Guide for the Diagnosis and Management of Skin and Soft Tissue Infections from the American Society for Infectious Pathologies.
In most cases the duration of oral treatment is 5 days. However, when no improvement is observed, treatment can be prolonged for periods of 10 to 14 days.
Hospitalization
There may be occasions when hospitalization of the patient is required for their best care. The following are some of these situations:
- Necrotizing infection.
- Signs of systemic toxicity or high fever.
- Immunosuppressed.
- Patients with poor adherence to medication and follow-up.
- Outpatient treatment fails.

Other support measures
Supportive therapeutic options are cold compresses, hydration, acetaminophen, or elevation of the lower extremities. Some studies have advised against the use of ibuprofen as a non-steroidal anti-inflammatory drug because of its likely effect in increasing the frequency and severity of necrotizing fasciitis.
When there is gangrene or abscesses in children, surgical debridement is required. Consequently, infants, the immunosuppressed, and the elderly should be admitted.
Considerations for erysipelas in childhood
In most cases, erysipelas in childhood is a disease with a good prognosis and is usually treated on an outpatient basis. That is, it responds favorably with oral antibiotics.
The diagnosis, as a general rule, is clinical, but if in doubt, the patient should be referred to a dermatologist. The specialist will be the one who indicates the treatment to be followed or the measures to be implemented. Therefore, you should not self-medicate in this type of pathologies under any circumstances.










